Studies have found that new lung cells can improve the treatment of cystic fibrosis

Studies have found that new lung cells can improve the treatment of cystic fibrosis

Copyright © iCell Bioscience Inc, Shanghai 2018-2019
Two research teams from the Boston area found that there is a new cell in the lung that has never been discovered before. Moreover, it may be associated with a serious lung disease.
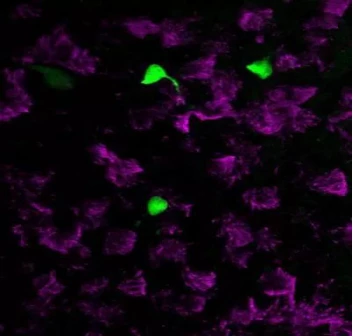
In the analysis, scientists accidentally found a new class of cells based on gene expression. Their CFTR gene expression levels were significantly higher compared to other cells. Under the fluorescence microscope, people first saw the true content of such cells. They look a lot like ionocytes on the surface of frog skin. Therefore, researchers simply refer to them as "pulmonary ionocytes.
Through single-cell sequencing techniques and efforts to compare cells, cells that were previously unknown were discovered.
Mucus is often found in the respiratory tract, and cells in the respiratory tract constantly remove these mucus. Through real-time imaging technology, the researchers found that these lung ion cells may be involved in this process.
As early as the 1980s, it was discovered that the protein encoded by this gene can participate in the transport of chloride ions on both sides of the cell membrane. If this gene is mutated, it will cause mucus accumulation in the lungs, pancreas, and other organs. In the lungs, this causes frequent respiratory infections, triggering a series of symptoms associated with cystic fibrosis. Cystic fibrosis is a serious multi-organ disease that affects more than 70,000 people worldwide.
Previously, the CFTR gene was thought to be expressed in ciliated cells common in the respiratory tract, but this study overturns this hypothesis. Subsequent studies have shown that the vast majority of CFTR proteins in the respiratory tract are expressed in these lung ion cells, and they account for only 1% of all cells.
Further studies have found that in the mouse model, typical phenomena of cystic fibrosis are caused by interfering with critical pathways in such cells. This finding indicates the important role of such cells in the pathogenesis of the disease, and it is expected that future gene therapy will be targeted and more precise.
When researchers developed new treatments for cystic fibrosis, knowing that only 1% of the cells needed to be used would bring many benefits, either to improve existing therapies or to help develop new therapies.
 Loading ....
Loading ....
