Research reveals a new mechanism for causing chronic sinusitis

Research reveals a new mechanism for causing chronic sinusitis

Copyright © iCell Bioscience Inc, Shanghai 2018-2019
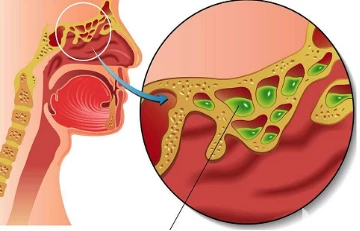
Chronic sinusitis is different from seasonal allergies. It causes inflammation and swelling of the sinuses for months to years, which causes breathing difficulties and other symptoms that can cause pain to the patient. In some people, chronic sinusitis also produces tissue growth called nasal polyp, and when the condition is severe, the nasal polyps must be surgically removed.
In a new study, researchers from the Massachusetts Institute of Technology and Brigham and Women's Hospital built the first of human barrier tissue during chronic sinusitis by performing genome-wide analysis of thousands of single cells from human patients. A global cell map. Analysis of these data suggests a new mechanism that may explain what maintains chronic sinusitis.
The findings also explain why some patients with sinusitis produce nasal polyps caused by airway epithelial cells. Research may have a broader impact on how scientists think about and treat other barrier tissue chronic inflammatory diseases such as asthma, eczema, and inflammatory bowel disease.
Researchers have developed a new portable technology that can rapidly sequence the RNA content of thousands of single cells from a small number of clinical samples in parallel. The technology, called Seq-Well, allows scientists to see which transcription programs are turned on in a single cell, giving them insight into the identity and function of these cells.
In this latest study, the researchers applied this technique to upper respiratory tract cells from patients with chronic sinusitis and speculated that different gene expression patterns in these epithelial cells may reveal why some patients develop nasal polyps. Other patients do not develop nasal polyps.
This analysis revealed significant differences in gene expression in basal epithelial cells (a tissue stem cell) from patients with chronic sinusitis with and without nasal polyps. In patients with chronic sinusitis and healthy people who do not develop nasal polyps, these cells usually form a flat layer of basal tissue covering the interior of the nasal cavity. In patients with chronic sinusitis who develop nasal polyps, these cells begin to accumulate and form thicker tissue layers rather than differentiate into subpopulations of epithelial cells required for host defense.
Scientists have observed this type of tissue abnormality for decades through histological experiments, but this new study reveals that basal cells from patients with chronic sinusitis that produce nasal polyps have initiated a specific gene expression program, which explains Their slow differentiation trajectories. This procedure appears to be directly maintained by IL-4 and IL-13, which are known to be over-produced at the pathological level of immune response cytokines that promote allergic inflammation.
The researchers found that these basal cells also retained their "memory" of exposure to IL-4 and IL-13: when they removed basal cells from non-nasal polyps and nasal polyps, they were cultured under the same conditions. One month, and then exposed to IL-4 and IL-13, it was found that unstimulated basal cells from patients with chronic sinusitis producing polyps have expressed many of them after induction in patients with chronic sinusitis without polyps. gene. Among the IL-4 and IL-13 responsive memory signals, a gene derived from a cell signal transduction pathway called Wnt that controls cell differentiation is included.
Immunologists have long known that B cells and T cells can store the memory of the allergens they have contacted, which explains why the immune system may overreact the next time it encounters the same allergen. However, these new findings have greatly increased the contribution of children and basal cells to this memory.
Given that as a stem cell, basal cells produce other cells found in the airway epithelium, this memory may affect their subsequent gene expression patterns and their ability to produce mature specialized epithelial cells. These researchers noted that the cell type balance in the airway epithelium of patients with severe disease was severely affected, which led to a reduction in the diversity of cell populations.
These findings suggest that efforts to block the effects of IL-4 and IL-13 may be a good way to try to treat chronic sinusitis. Against this hypothesis, these researchers used antibodies that block the same receptor for both cytokines. This antibody has been approved for the treatment of eczema and is being tested for other uses.
The researchers analyzed genes expressed in basal cells obtained from a patient with chronic sinusitis who developed nasal polyps before and after receiving this antibody treatment. The researchers found that most of the genes activated by IL-4 and IL-13 (but from time to time all genes) have returned to normal expression levels. This suggests that blocking IL-4 and IL-13 helps restore basal and secretory cells to a healthier state, but there is still some residual genetic trait.
These researchers are now planning further detailed analysis of how the basal cells store the molecular mechanisms of inflammatory memory, which may help them discover other drug targets. Inflammatory diseases affecting other parts of the body, such as inflammatory bowel disease, are also being studied, in which inflammation usually causes polyps that may become cancer.
Studying whether stem cells in the gut may also remember immune events, maintain disease, and play a role in tumor formation will be key to developing early interventions for inflammation-induced cancer.
 Loading ....
Loading ....
